How Can You Get Tested for Osteoporosis? Discover the Essential Steps
Have you ever wondered how to maintain strong, healthy bones as you age? Osteoporosis might not cross your mind until you or a loved one experiences a fracture. This silent disease, characterized by brittle bones, can progress without noticeable symptoms until a break occurs. But how can you test for osteoporosis, and why is it important to get tested? Let’s embark on a journey to understand the process and ensure your bone health remains in check.
Understanding Osteoporosis: The Silent Bone Thief
Osteoporosis occurs when the cycle of bone breakdown and regeneration becomes imbalanced. As our bodies age, bone mass and density naturally decline. When the bones become porous and fragile, the risk of fractures escalates, even from minor falls or injuries.
Key Risk Factors for Osteoporosis
While aging is a significant factor, other conditions and lifestyle factors can increase the likelihood of developing osteoporosis:
- Gender: Women, especially post-menopausal, are more at risk.
- Family History: A familial history of osteoporosis can predispose individuals.
- Body Frame Size: Smaller body frames tend to have higher risks because they may have less bone mass.
- Hormonal Levels: Low estrogen levels in women or low testosterone in men can contribute.
- Dietary Habits: A diet lacking in calcium and vitamin D can exacerbate bone thinning.
- Lifestyle Choices: Smoking, excessive alcohol use, and a sedentary lifestyle can also heighten the risk.
Recognizing these risk factors is a crucial step in understanding why you might need to get tested for osteoporosis.
The Process of Getting Tested: What to Expect
Wondering what the journey entails when considering osteoporosis testing? Here’s what you need to know.
When to Consider Osteoporosis Testing
Experts recommend testing for:
- Women aged 65 and older, and men aged 70 and older, regardless of risk factors.
- Postmenopausal women and men aged 50-70 with risk factors.
- Individuals who experience a bone fracture after age 50.
- Those who have a condition or take a medication associated with bone loss.
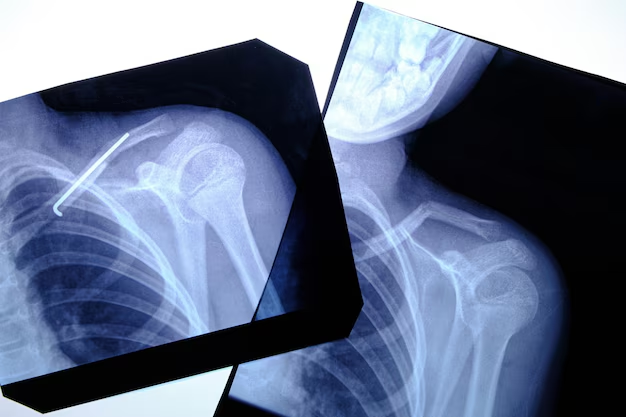
The Bone Density Test: Dual-Energy X-ray Absorptiometry (DEXA or DXA)
The most common and efficient test for diagnosing osteoporosis is the DXA scan. This painless procedure involves:
- Positioning: You lie on a padded table, while the scanner passes over your lower spine and hip, analyzing bone density.
- Duration: The procedure typically takes about 10 to 30 minutes.
- Safety: It involves very low levels of radiation, much lower than a chest X-ray.
Understanding DXA Scan Results
After your DXA scan, you’ll receive a T-score, which compares your bone density to a healthy 30-year-old. Here’s how to interpret your results:
- Normal Bone Density: T-score of -1.0 and above.
- Low Bone Density (Osteopenia): T-score between -1.0 and -2.5.
- Osteoporosis: T-score of -2.5 and below.
Your healthcare provider will discuss these results, considering other factors like your medical history and risk variables.
Beyond the DXA: Other Diagnostic Methods
While the DXA scan is the gold standard, other tests can complement osteoporosis diagnosis.
Additional Imaging Tests
- Quantitative Computed Tomography (QCT): Provides a 3D image for more detailed information on bone density, but involves higher radiation.
- Ultrasound: Used on peripheral sites like the heel, it provides quick results and involves no radiation, though it’s not as detailed as DXA.
Blood and Urine Tests
These tests help assess bone turnover and rule out secondary causes of osteoporosis. They can also monitor response to osteoporosis treatment:
- Calcium and Vitamin D Levels: Indicates if you need dietary adjustments.
- Thyroid Function: Imbalances can affect bone density.
- Parathyroid Hormone Levels: Hyperparathyroidism can lead to bone loss.
The Role of Healthcare Providers in Osteoporosis Testing
Your healthcare provider plays an essential role in guiding you through the testing and diagnostic process. Here’s how they can assist:
- Risk Assessment: Evaluating personal and family medical history.
- Test Recommendations: Advising the most suitable tests based on your risk and symptoms.
- Interpreting Results: Helping you understand your bone density scores and potential steps forward.
Taking Action: Prevention and Lifestyle Modifications
Testing for osteoporosis is just one aspect of managing bone health. Proactive steps can significantly mitigate the risk of osteoporosis and its complications.
Prioritize Nutrition
Ensuring your diet is rich in calcium and vitamin D is fundamental:
- Calcium Sources: Dairy products, green leafy vegetables, and fortified cereals.
- Vitamin D: Sunlight exposure, fatty fish, and supplements if necessary.
Physical Activity Focus
Engage in weight-bearing and resistance-training exercises:
- Walking, Jogging, Dancing: Activities that force you to work against gravity.
- Strength Training: Builds muscle strength, supporting bone health.
Lifestyle Modifications
Adopt habits that foster bone health:
- Quit Smoking: Smoking cessation can improve bone density.
- Limit Alcohol: Keeping alcohol consumption to moderate levels benefits bones.
Medication Management
For those diagnosed with osteoporosis, several treatments can reduce fracture risk:
- Bisphosphonates: Often the first line of treatment.
- Denosumab: An injection that helps increase bone density.
- Hormone-Related Therapy: For menopausal women, estrogen replacement can be beneficial.
Regular Monitoring
Regular follow-up appointments can help track your bone health, ensuring timely interventions if your condition changes. Discuss with your healthcare provider about how frequently you need repeat tests based on your risk factors.
Empowering Yourself with Information
Understanding the process of getting tested for osteoporosis puts you in control of your health. Knowledge about risk factors, available testing methods, and preventive strategies can set you on a path to maintaining strong, resilient bones.
Whether you’re in a high-risk category or interested in preventive care, staying informed and proactive about bone health will make all the difference. Don't wait for a fracture to raise the red flag—engage with your healthcare provider about osteoporosis testing today.
Summary: Your Osteoporosis Testing Guide 🚦
- Recognize Risk: Aging, gender, family history, and lifestyle choices contribute to osteoporosis.
- Seek Testing: Consider testing if you're a woman over 65, a man over 70, or at risk.
- DXA Scan: Painless, quick bone density test with minimal radiation.
- Results Interpretation: Understand T-scores; normal, osteopenia, or osteoporosis.
- Additional Tests: Consider QCT, ultrasound, blood, and urine tests.
- Healthcare Support: Consult professionals for tailored advice and risk assessment.
- Lifestyle Focus: Maintain nutrient-rich diet, engage in physical activity, and modify lifestyle habits.
- Stay Informed: Regular monitoring and proactive engagement with your healthcare provider ensure optimal bone health.
Related Articles
- a Nurse Is Caring For a Client Who Has Osteoporosis.
- a Percutaneous Is Performed To Treat Osteoporosis Related Compression Fractures
- Can Alcohol Cause Osteoporosis
- Can I Do Pilates If I Have Osteoporosis
- Can I Reverse Osteoporosis
- Can Men Get Osteoporosis
- Can Osteoporosis Affect Teeth
- Can Osteoporosis Be Cured
- Can Osteoporosis Be Painful
- Can Osteoporosis Be Reversed
