Understanding Tuberculosis: How It Spreads and What You Can Do About It
Every year, millions of people across the globe are affected by a microbial adversary, an insidious bacterium that targets the lungs. But how exactly does tuberculosis (TB) spread, and what measures can we take to protect ourselves? Let’s delve deeper into understanding tuberculosis transmission and explore steps to mitigate its spread.
What is Tuberculosis?
Tuberculosis is a potentially serious infectious disease primarily affecting the lungs, although it can impact other parts of the body. It’s caused by the bacteria Mycobacterium tuberculosis. Unlike some other bacterial infections, TB spreads primarily through the air, a fact that underscores the importance of understanding its transmission to prevent it effectively.
How is Tuberculosis Spread?
The Airborne Nature of TB
Tuberculosis is predominantly an airborne disease. When a person with active pulmonary TB coughs, sneezes, laughs, or speaks, tiny droplets containing TB bacteria are expelled into the air. These droplets can be inhaled by others, leading to the spread of the infection.
Factors Influencing Transmission
Several factors can influence how TB spreads, including:
- Infectiousness of the Individual: A person with active TB in the lungs or throat is the primary source of infection.
- Environment: Unventilated, crowded spaces increase the likelihood of transmission.
- Duration of Exposure: Prolonged contact with an infected person raises transmission risk.
- Immune System of the Person: Individuals with weakened immune systems, such as those with HIV, are more susceptible to TB infection.
Understanding these factors highlights the importance of timely diagnosis and treatment to prevent further spread.
Who Is at Risk for TB?
While anyone can contract TB, certain groups are more vulnerable:
- People with weakened immune systems, including those with HIV/AIDS, are more susceptible to developing active TB.
- Individuals living in close quarters where someone has active TB, such as households or places with poor ventilation.
- Healthcare workers due to exposure to patients with TB.
- People in regions with high TB prevalence, typically in parts of Africa, Asia, and Eastern Europe.
Stages of TB: Latent vs. Active
Understanding TB fully requires differentiating between its two stages:
Latent TB Infection (LTBI)
In latent TB infection, a person has the TB bacteria within their body, but it remains inactive and causes no symptoms. Importantly, individuals with LTBI cannot spread the bacteria to others. However, without treatment, about 5-10% of these individuals may eventually develop active TB.
Active TB Disease
Active TB occurs when the bacteria become active in the body, leading to symptoms and the potential to spread the disease to others. Symptoms might include a persistent cough, chest pain, fatigue, fever, night sweats, and weight loss. Recognizing active TB symptoms early is crucial for preventing its spread.
Preventing TB Transmission
Effective Measures to Reduce Risk
- Prompt Diagnosis and Treatment: Identifying and treating active TB cases quickly is vital for controlling transmission.
- Ventilation: Ensuring good air circulation in homes and workplaces can minimize the risk of transmission.
- Respiratory Hygiene: Covering mouth and nose when coughing or sneezing can reduce the spread of TB bacteria.
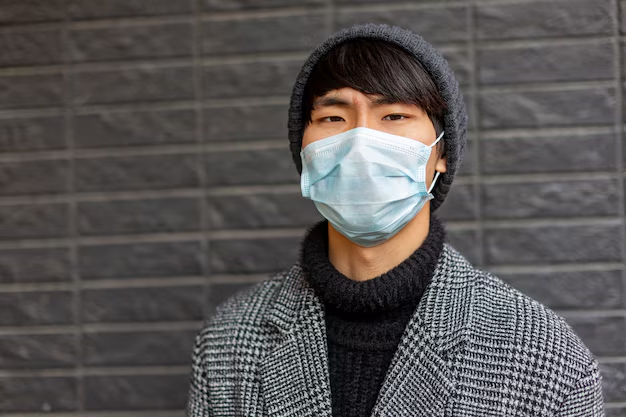
- Use of Masks: High-risk individuals, including healthcare workers, might use masks to protect themselves from inhaling bacteria.
Vaccination: The Role of BCG
The Bacillus Calmette-Guérin (BCG) vaccine provides protection against TB, particularly in children. Although it doesn’t prevent COVID-19, it guards against severe forms of TB like meningitis in young ones. The vaccine's impact on adults is less consistent. However, it remains a crucial tool in TB prevention strategies worldwide.
What to Do If You Suspect Exposure
Getting Tested
If you've been in contact with someone who has TB or if you exhibit symptoms, getting tested is a prudent step:
- Tuberculin Skin Test (TST): Also known as the Mantoux test, this involves an injection in the forearm, checked by a healthcare professional after 48-72 hours for a reaction.
- Interferon Gamma Release Assays (IGRA): This blood test can detect TB infection by measuring the immune response to TB bacteria.
Navigating Test Results
A positive TB test doesn’t always indicate active disease. Your healthcare provider may suggest further examinations like chest X-rays or sputum tests to ascertain whether you have latent or active TB.
The Importance of Treatment
Treatment for Latent TB
Preventing latent TB from developing into active TB involves medication, typically isoniazid or rifampin, aim to eliminate dormant bacteria.
Treating Active TB
Treatment for active TB is more intensive and requires a combination of antibiotics over 6-9 months. Adherence to the treatment regimen is crucial to prevent drug resistance and ensure recovery.
Supporting Global TB Control
Though TB is prevalent in certain areas, efforts to control it must be global. Organizations like the World Health Organization work relentlessly to improve access to testing and treatment services, especially in high-burden regions.
How You Can Help
- Spreading Awareness: Educating others about TB transmission and symptoms.
- Supporting Public Health Initiatives: Engage with programs aimed at reducing TB's impact.
- Encouraging At-Risk Individuals to Get Tested: Early detection is a cornerstone of TB control.
Challenges in TB Control and Future Directions
Drug-Resistant TB
A growing challenge in treating TB is drug-resistant strains, which do not respond to conventional treatments. Addressing this requires new medications and treatment strategies.
Innovations in TB Testing and Treatment
Research into new diagnostic tools and shorter, more effective treatment regimens holds promise in the fight against TB. Enhanced vaccines and more accessible treatment options are key components of future TB control efforts.
The path towards eradicating tuberculosis is driven by education, awareness, and collective actions on personal and global levels. Understanding how TB spreads and recognizing symptoms are pivotal steps towards healthier communities.
Key Takeaways:
- 🌬 TB spreads through the air—primarily from person to person.
- 👥 High-risk groups include those with weakened immune systems and close contacts with infected individuals.
- 💉 Vaccination and prompt treatment help prevent and control TB.
- 🔍 Testing is crucial if TB exposure is suspected.
- 🌎 Collective global efforts are vital to combat the disease.
By staying informed and supportive of public health measures, we all play a crucial role in defeating tuberculosis, one step at a time.